Lupus Facts: Types, Causes, Symptoms, Diagnosis, and Treatment for Lupus
Lupus, otherwise referred to as systemic lupus erythematosus is an autoimmune disorder that affects the body resulting in pain and edema. An autoimmune disease, simply means that the immune system of the body is attacking itself rather than fighting against only pathogens (2). As a result of its complex immune manifestation, lupus is otherwise referred to as the disease of a thousand faces (3).
Per lupus facts and statistics from the Lupus Foundation of America, at least five million people worldwide and about 1.5 million Americans, have some form of lupus. Out of these, maximum percent of people with lupus are women.
Lupus symptoms include pain, fatigue, hair-loss, cognitive issues, and physical impairments. People with lupus may also suffer from cardiovascular disease, strokes, rashes, and pain in their joints. And there may be no visible symptoms for others.

It is often difficult to make a diagnosis of lupus because it has non-specific symptoms that look like other agents. The butterfly rash on the face is pathognomonic of lupus but not all patients give the classical symptoms. Unfortunately, there is currently no cure for lupus, patients with lupus can only be managed (1).
Lupus Facts: Types Of Lupus
There are quite a several kinds of lupus. Of all, systemic lupus erythematosus is the commonest.
- – Systemic lupus erythematosus
This is the commonest type of lupus and it consists of approximately 70 percent of cases recorded. Being systemic, multiple organs of the body are at risk and due to this, SLE is the most severe lupus in clinical practice.
Systemic lupus can affect the joints, the kidneys, and the blood. Other areas that can be affected are the skin, and the heart, and the inflammation is capable of affecting multiple organs at the same time.
SLE is associated with active and remission phases. During the active phase, the patient manifests signs and symptoms of the disease and during remission, the patient is asymptomatic, and the cycle continues like that (3).
- – Cutaneous lupus erythematosus
Cutaneous lupus majorly affects the skin of the affected individual. Patients presenting with cutaneous lupus present with symptoms of hypersensitive skin, sunburns, skin rashes, and sometimes they have alopecia, meaning hair loss (2).
- – Drug-induced lupus
Certain medications can predispose a person to lupus and such is referred to as drug-induced lupus, and it disappears once the patient stops such medications. It has clinical features similar to systemic lupus erythematosus but it has a brief duration of illness (2).
- – Discoid lupus erythematosus
The discoid lupus erythematosus is another type of lupus with cutaneous manifestation. It is characterized by the appearance of a skin lesion usually on the face and scalp of the patient, and this lesion is usually circular. Unfortunately, they can also affect some inner ears which may not be noticed early.
It usually results in discoloration of the skin and leaves scars after treatment. When discoid lupus affects the scalp, hair usually does not grow back in the affected scalp areas. Studies revealed that about 10 percent of patients with DLE, later develop systemic lupus later in life (3).
- – Neonatal lupus
Neonatal lupus is a rare form of lupus seen in a newborn at birth. Studies have shown that it is a result of antibodies detected in the infants which are believed to be inherited from their mothers who had lupus with pregnancy or the children might have solely developed the condition. Not every woman who had lupus with pregnancy will end up having a child with neonatal lupus (2).
Neonatal lupus manifestation includes skin diseases, anemia in children, and hepatic (liver) diseases. The skin features may completely disappear after weeks but this is dependent on the severity of the disease, and sometimes some children have congenital heart diseases that will require the use of assisted devices such as a pacemaker to regulate the heart (3).
- – Lupus nephritic
Lupus nephritic is a type of lupus resulting from the affection of the kidneys by systemic lupus erythematosus. Patients with lupus nephritic have the clinical manifestations of kidney disease (4).
Who Is Affected By Lupus?
Lupus onset age is non-specific as anyone can be affected. Both genders are at risk of lupus as it is not gendered specific but it is commoner in women than men, especially women of reproductive age group (2).
It is very rare for lupus to occur before the age of 5 years but studies reveal that about 20 percent of lupus are seen before 20 years of age. Nephritic lupus affecting the kidneys is also commonly seen in children with more severe manifestations (3).
A lot of cases of lupus go undiagnosed because of similarity in manifestation to other medical conditions.
It is commoner among African-American, Asian, and Hispanic women. It is less common among Caucasians. A family history of lupus predisposes more to the disease (2).
Lupus Facts: Causes Of Lupus
The exact cause of lupus is currently unknown. But, there are identified factors that are known to predispose individuals to lupus. The possible factors are:
- – Genetics or family history
Although researches are still in progress studies have revealed that certain genes predispose an individual to develop lupus. Family history is also a non-modifiable risk factor for developing lupus because of the high tendency of having the disease if it is already present in a family member, especially first-degree relatives.
There is also a 24 percent chance of infection in monozygotic twins in developing lupus. It is important to note that lupus can also occur in people who have a family history of other autoimmune diseases aside from lupus (3)
There are also evidences that lupus is more present in certain ethnic denomination than the others like Native American, Hispanics, Asians, and others which may also strengthen the explanation of genetics being a factor (4).
- – Environmental factor
Certain things in the environment make some people at more risk of developing lupus. Factors such as sunlight, atmospheric microorganisms like viruses, smoking, and even stress predispose an individual to lupus (2).
The possible environmental factors are:
- * Sunlight: Excessive exposure to sunlight worsens the condition of patients with systemic lupus erythematosus but researches are still ongoing if this causes lupus on its own.
- * Smoking: Cigarette contains some toxic chemicals which are capable of altering the genetic changes of individuals. However, these genetic activations have been traced to SLE
- * Infections: Glandular fever caused by the Epstein-Barr virus has been traced down to one of the features seen in patients with SLE. However, individuals at risk of lupus who are solitarily infected by glandular fever are then more predisposed to SLE.
- * Air pollution: In industrialized areas where passive smoking is rampant, individuals at risk of lupus can come down with the disease as a result of the toxic chemicals in the smoke (3).
- – Hormonal factors
The onset of lupus in most women is associated with a period of high estrogen release. And that is why women commonly develop lupus before their monthly flow or during the period of pregnancy. Interestingly, medications that seem to contain estrogen-like birth control pills do not put women at risk of lupus. Researches are currently ongoing regarding the cause of this (4).
- – Drugs
Certain medications predispose an individual to develop lupus. Examples of such are procainamide and hydralazine. Fortunately, there is a resolution of the disease symptoms once the patient stops the use of such drugs. But, on rare occasions, symptoms can persist even after the patient stop taking the medications (4).
Lupus Facts: Signs And Symptoms Of Lupus
Different patients will not necessarily manifest the same signs and symptoms as no two patients have the same manifestations. The manifestations in individuals differ in onset, severity, and duration. The symptoms also have periods of flares when they are very active and, remissions when they subside.
The clinical manifestations in patients with lupus are dependent on which system of the body is affected (1).
The general signs and symptoms of lupus are:
- – tiredness,
- – joint pain,
- – hypersensitivity to light,
- – a butterfly rash on the face and nose called malar rash,
- – mouth ulcers,
- – difficulty in breathing,
- – chest pains, and
- – slow mentation.
- – others are headaches, alopecia (hair loss), depression, confusion, and fever (3).
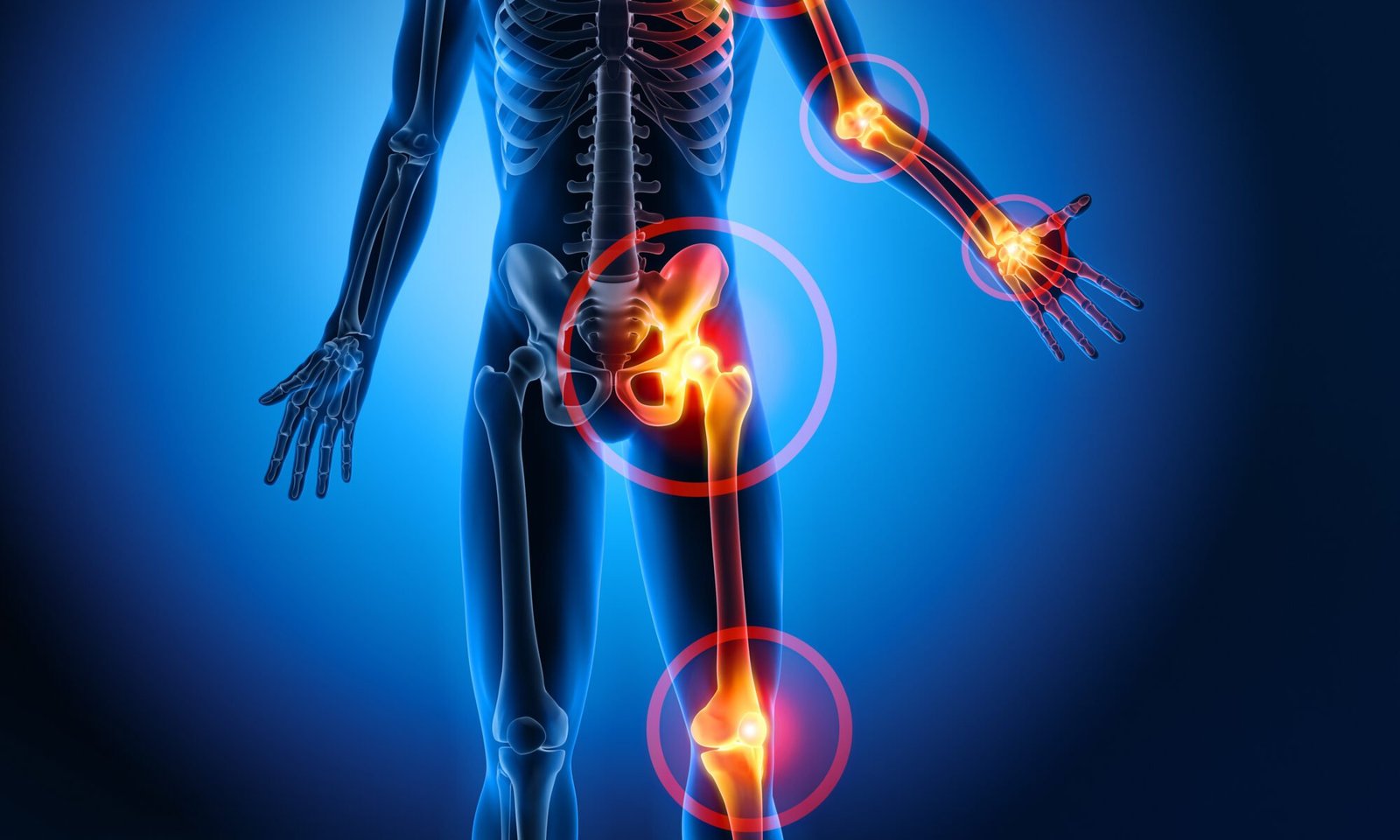
Facts About Lupus: Effects Of Lupus On The Body
The effects of lupus are widespread in the body and so many organs can be affected at the same time. It often results in body pains and most times severe complications. The parts of the body commonly affected by the autoimmune disease, lupus are the skin, joints, and kidneys. Other parts of the body that can be affected are the blood, the heart, and the lungs (2).
- – Skin
The skin is one of the commonest sites for the manifestation of lupus disease. Patients with lupus have the butterfly, malar rash over their face and bridge of the nose. Other skin issues that can result are discoid rash (red rash with scales and plaques commonly around the ears, the scalp, and the forehead.), hair loss, sores, and scars from previous rashes. Exposure to sunlight complicates the skin rashes (2)
- – Kidneys
When lupus affects the kidneys, it is called nephritic lupus. It results in inflammation of the nephrons of the kidneys preventing the kidneys from functioning properly. Some of the symptoms include leg swelling and early morning facial puffiness, the frothiness of the urine (foaming), and elevated blood pressure (3).
- – Heart
When lupus affects the heart, it results in inflammation of the layers of the heart causing myocarditis when it affects the muscles of the heart and endocarditis when it affects the inner layer of the heart. Patients present with symptoms such as chest pain and sometimes difficulty in breathing. Endocarditis can get complicated and result in a hole in the heart (3).
- – Blood
Lupus is also capable of affecting the blood. It can cause a decrease in the number of blood vessels resulting in anemia or reduced white blood cells called leukopenia. When it affects the platelets and reduces their number, it is called thrombocytopenia (3).
- – Joints
Patients with lupus are at risk of arthritis in the joints. This usually manifests as edema and pain in the affected joint. Sometimes, the patient can also complain of joint stiffness which is worse early in the morning. Arthritis as an effect of lupus can appear and resolve after a while but sometimes it doesn’t (4).

- Lupus versus rheumatoid arthritis
Both lupus and rheumatoid arthritis are autoimmune diseases affecting the joints. Comparing lupus vs ra, kidney problems, rashes, and joint pains are more common with systemic lupus erythematosus compared to rheumatoid arthritis, and the joint involvement is more severe in rheumatoid arthritis than lupus. But, both present with joint stiffness and swelling (7).
- – Pregnancy
It is possible to have an uneventful pregnancy with lupus. But, women having lupus with pregnancy are more at risk of complications in pregnancy (6). Such women need to start making preparations with their gynecologist and obstetricians even before the pregnancy journey starts because lupus with pregnancy is a high-risk pregnancy.
The risk of complication is much higher for women having lupus with pregnancy who have other co-morbidities like diabetes, high blood pressure, kidney diseases, and low platelet count. Flares are not uncommon in pregnancy but are commoner during the first and second trimesters (5).
Lupus Facts: Diagnosis Of Lupus
The following lupus test results are important in making a diagnosis of lupus.
- – Anti-Nuclear antibody (ANA)
The anti-nuclear antibodies are present in the nuclei of the human cells. The majority of patients with lupus are going to test positive for the ANA test. It is seen as the confirmatory or definitive diagnostic test for lupus.
The ANA blood test shows patterns and the patterns are important in the treatment of the disease. For example, the diffuse pattern is restricted to patients with SLE. Other patterns available are peripheral, speckle, and nucleolar patterns. Rarely, there are cases of lupus with negative ANA but this is seen in only about 2 percent of reported cases, but such patients can have antiphospholipid antibodies (8).
- – Anti-dsDNA Antibody
This is another type of antibody for ANA, and it can be seen specifically in about thirty percent of patients with systemic lupus.
- – Anti-Ro/SSA
This antibody is mostly seen in lupus patients who are not reactive to the anti-nuclear antibody (8).
Lupus Facts: Treatment For Lupus
The treatment of lupus involves the use of both medications and lifestyle changes.
Below are medications important for the treatment of lupus:
- – Hydroxychloroquine: This medication assists with the treatment of arthritis and skin rashes that result from lupus
- – Corticosteroids: An example of this drug is oral prednisolone to help resolve inflammation and suppress the activity of the immune system
- – Belimumab: This drug has newly been approved for the treatment of lupus (3).
The lifestyle changes required in the management of lupus are adequate exercise and rest, proper stress management, stopping smoking, and taking less alcohol (3).
References:
- 1. https://www.mayoclinic.org/diseases-conditions/lupus/symptoms-causes/syc-20365789#:~:text=Overview,%2C%20brain%2C%20heart%20and%20lungs.
- 2. https://my.clevelandclinic.org/health/diseases/4875-lupus
- 3. https://www.medicalnewstoday.com/articles/323653
- 4. https://www.webmd.com/lupus/arthritis-lupus
- 5.https://www.cdc.gov/lupus/basics/pregnancy.htm#:~:text=Women%20with%20lupus%20can%20safely,likely%20for%20women%20with%20lupus.
- 6. https://www.lupus.org/resources/planning-a-pregnancy-when-you-have-lupus
- 7. https://www.medicalnewstoday.com/articles/lupus-vs-ra
- 8. https://www.hopkinslupus.org/lupus-tests/lupus-blood-tests/#:~:text=It%20is%20possible%20for%20people,Ro%2FSSA%20or%20antiphospholipid%20antibodies.